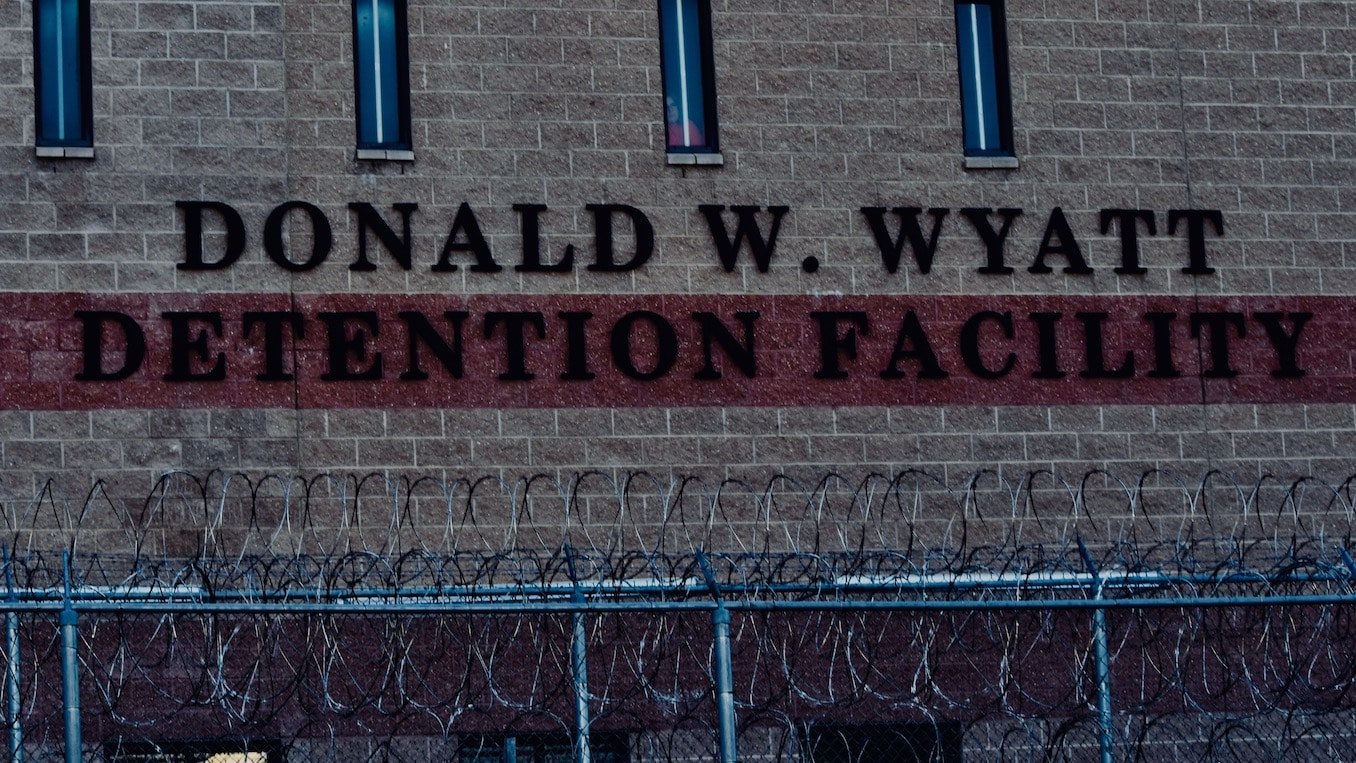
COVID-19 cases have exploded at the Wyatt; Is the ACI next? State officials say no…
“We’ve tested all the workers, all the inmates,” said Governor Gina Raimondo at Friday’s COVID-19 press briefing. “We’ll continue to do that on a somewhat cyclical basis. We’re doing our best to isolate folks. We have an excellent care team there. We’ve been better able to provide PPE to everybody there. I think we have a comprehensive plan.“ As of
May 19, 2020, 10:43 am
By Steve Ahlquist
“We’ve tested all the workers, all the inmates,” said Governor Gina Raimondo at Friday’s COVID-19 press briefing. “We’ll continue to do that on a somewhat cyclical basis. We’re doing our best to isolate folks. We have an excellent care team there. We’ve been better able to provide PPE to everybody there. I think we have a comprehensive plan.“
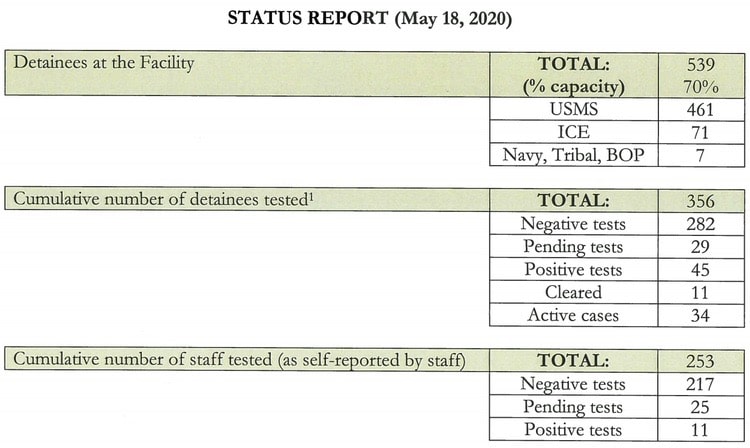
As of yesterday’s report, filed by the Wyatt Detention Facility per a court order, there are 34 active cases of COVID-19 among the prisoners, and 11 additional prisoners have tested positive but have since been cleared of the disease. 11 members of the Wyatt staff have also tested positive.
Meanwhile, at the Adult Correctional Institutions (ACI) three asymptomatic inmates in Minimum Security have tested positive, and seven members of the staff at the ACI have tested positive, putting the ACI, today, where the Wyatt was about a month ago when it comes to the pandemic.

So will we be seeing numbers at the ACI in June similar to what we’re seeing at the Wyatt today?
No, says Rhode Island Governor Gina Raimondo and Rhode Island Department of Health (RIDOH) Executive Director Dr Nicole Alexander-Scott.
“We’ve tested all the workers, all the inmates,” said Governor Raimondo at Friday’s COVID-19 press briefing. “We’ll continue to do that on a somewhat cyclical basis. We’re doing our best to isolate folks. We have an excellent care team there. We’ve been better able to provide PPE to everybody there. I think we have a comprehensive plan.”
Dr Nicole Alexander-Scott explained further:
“The testing process has been focused on where we are seeing the outbreak. [There are a number of reasons] why we are not anticipating, three to four weeks from now, having a repeat of what we’ve seen [at the Wyatt],” said Dr Alexander-Scott. “One is this was a proactive, comprehensive, aggressive approach at assessing what the risk of spread is. These [tests] weren’t [conducted based on] the fact that there [was] someone who was symptomatic and then it had spread and by the time we found out it was too late. This was in advance of any of that occurring. We actually went in to do the type of testing [that would] help us understand and determine [whether] are we at risk of something like that happening.
“That wasn’t the case in Wyatt when we were there. We’re going to continue that process as we go forward as we have been doing in all of the congregate care settings and we’ll get to the place where we’re able to assess that for all of the inmates and all of the staff.
“The other reason is what the governor mentioned. We have an excellent leadership and medical care team at the Department of Corrections that we work very closely with,” continued Dr Alexander-Scott. “They have done a phenomenal job up until now, even knowing that this was not just the reactive process of a cluster of cases. This was us going there, proactively looking to see how can we help prevent some form of cluster of cases or challenge from occurring. So we really credit the leadership there in Director Patricia Coyne-Fague as well as Dr Jennifer Clarke, who have done an excellent job with a huge team there.”
The Wyatt report noted that it has been working with RIDOH and CSST (Congregate Settings Support Team) to improve its response to COVID-19:
Quarantine and Testing Procedures
With the input of RIDOH and the CSST, the Facility’s current intake and
quarantine procedures are as follows:
- The Facility uses J-1 Pod (“J-1”) and F-Pod as the intake pods for all new detainees from the United States Marshals Service, ICE, the Federal Bureau of Prisons, and the United States Navy;
- J-1 is the Facility’s primary quarantine pod and can house up to 48 detainees. The Facility intends to use F-Pod (16 beds) as supplemental location for new detainees if J-1 is full or the Facility needs to use F-Pod to maintain its cohorting arrangements within J-1;
- J-1 and F-Pods are separate and smaller units within the Facility;
- The Facility selected J-1 and F-Pod as the most appropriate spaces for quarantine given their size, layout, and location within the Facility;
- The Facility uses J-1 and F-Pod as initial intake holding pods to assess and clear detainees before releasing them into the general population;
- Although the Facility currently has two medical isolation units which are negatively pressured, the Facility’s HVAC contractor has successfully completed work to turn the entire J-1 pod (48 beds) into a negative pressure isolation unit and, as of May 8, 2020, the entire I-Pod (female detainees, 40 beds), and the entire K-Pod (special purpose/protective custody, 70 beds) are negatively-pressured;
- The Facility screens new detainees by asking them questions regarding their travel history, contact with potential COVID-19 positive individuals, and other risk and exposure factors;
- All detainees arriving to the Facility are held in isolation, medically screened, and tested for COVID-19 on the third day after their arrival;
- This lockdown consists of being isolated into a single-person cell and separated from all other interaction with detainees in their pods. Quarantined detainees are permitted to leave their quarantine cells alone up to one hour per day to shower, recreate, and to make one phone call;
- Detainees in J-1 and F-Pod are monitored and medically screened daily, and mental health unit staff check in with the J-1 and F-Pod detainees every day the staff are onsite;
- During this period, detainees are instructed to self-report any symptoms;
- If the detainee’s initial test is negative, the Facility waits four additional days and then re-tests the detainee;
- If, after this eight-day period there are two negative tests, then the detainee will be cleared for release into the general population;
- If a new detainee receives a positive test during this initial quarantine period, the detainee will remain in isolation in the Facility’s negative pressure unit, closely monitored for symptoms, and re-tested;
- Only after two successive negative tests will the detainee’s condition be considered resolved or cleared;
- Any detainee who refuses medical screening is not moved to general population but is instead issued a disciplinary ticket and placed into segregation; and
- To date, no detainee has refused COVID-19 related medical screening.