Nursing home resident and caregiver COVID-19 deaths surpassed 1,000 this week
“Every day nursing home residents and frontline heroes are dying from COVID-19 yet the industry continues to obscenely claim they can’t afford the staffing and support needed to help contain the spread,” continued Adanjesus Marin, Coordinator of Raise the Bar on Resident Care.
December 17, 2020, 2:35 pm
By Steve Ahlquist
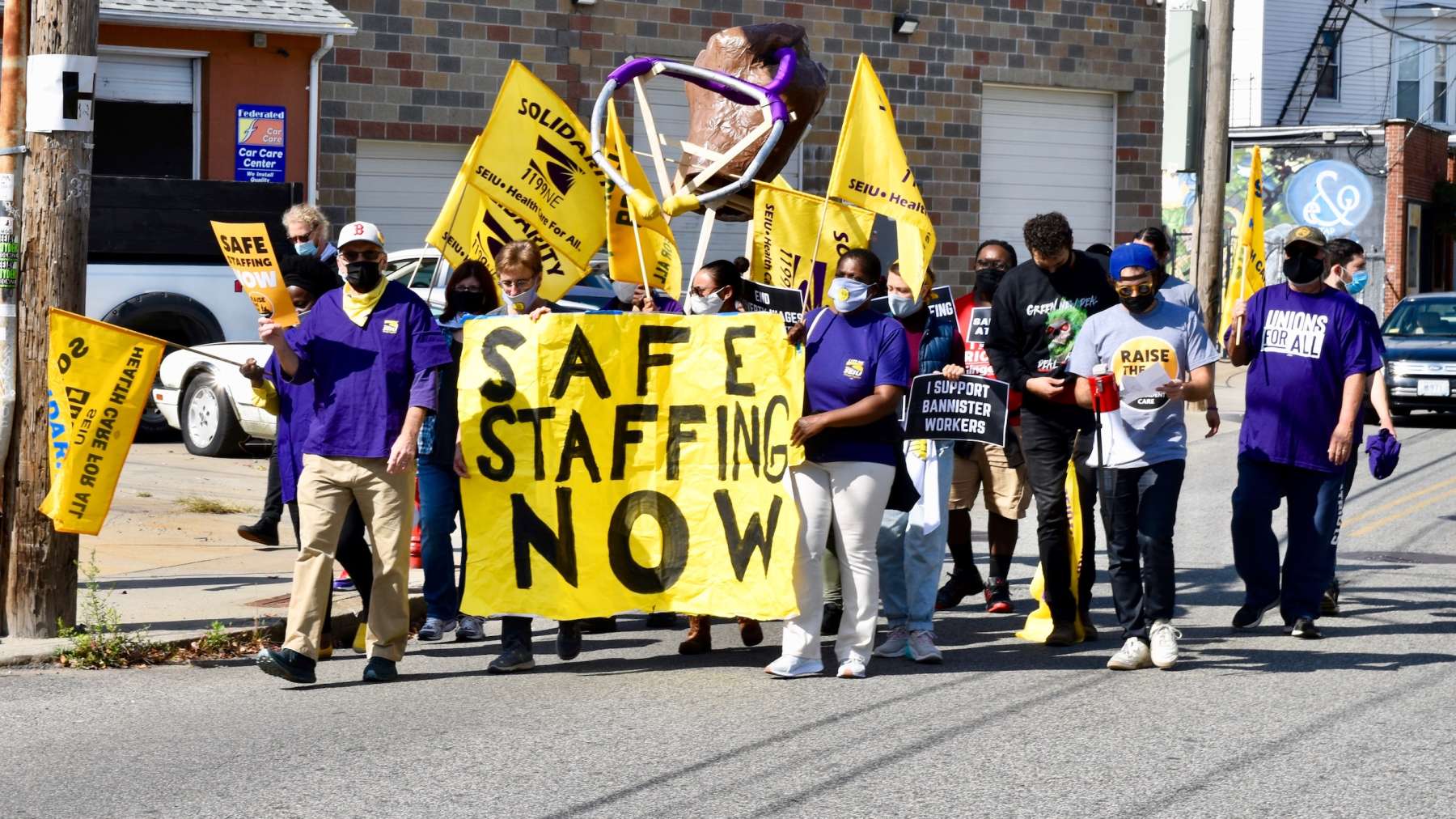
Rhode Island is one of three states (with New Hampshire and Connecticut) where long term care COVID-19 deaths account for over 70% of all COVID-19 deaths. The national average is 40%. How many nursing home caregivers have died to Covid is unknown, since the state doesn’t seem to track or publish that data. In response, the state has been slow to enact policies to ensure adequate staffing levels at nursing homes, putting workers and residents at risk.
“Nursing home heroes and our state’s most vulnerable citizens have been the victims of dangerously low short staffing for decades – the pandemic is pushing them to a breaking point,” said Adanjesus Marin, Coordinator of Raise the Bar on Resident Care. “There is a direct correlation between staffing levels and infection control violations yet the industry continues to claim they are powerless to stop the spread. It is time our elected officials hold industry leaders accountable to keeping nursing home residents and caregivers safe as their lives are put at risk daily.”
Nationally, Rhode Island ranks 41st in the nation for the average number of hours of care residents receive each day. Multiple studies show that higher staffing means lower rates of Covid infection. In Rhode Island, front-line caregivers struggle o care for 10-15 patients each, many who are critically ill with Covid.
“The pandemic has been absolutely heartbreaking – I left work every day crying because I felt I couldn’t do enough to save residents dying from COVID-19,” said Stefania Silvestri, a registered nurse at RN, works at Greenville Center where up to 79 residents became ill with COVID-19 and at least 20 have died. “Because of short staffing, we had to body bag our own residents and many caregivers and their families contracted the virus, including myself and my husband who lost his job and our medical benefits. And as COVID-19 cases surge again, nothing has changed – we still don’t have the staffing we need to keep us safe.”
Rhode Island Governor Gina Raimondo this week announced that the Rhode Island Department of Health will be mandating “‘3.8 staff hours per resident per day’ for nurses, CNAs and other direct care workers.”
“We think that would be a significant step forward,” said Marin, “while we continue to advocate for the passing of our legislation in the General Assembly.”
The nursing home industry is crying poverty in response to Governor Raimondo’s announcement, and claims that increased staffing “will put a number of homes out of business.” The industry says this despite having earned $241m in profit in 2017-18. These same nursing homes received over $60 million in additional state and federal funding since April 1 to support increased staffing, testing and PPE. According to Skilled Nursing News, “the new Medicare payment model for nursing homes provided $200 more per day than the system it replaced in October 2019. That works out to about $90,000 extra in bottom-line revenue each month for a facility with an average of 15 Medicare residents each day.”
“Every day nursing home residents and frontline heroes are dying from COVID-19 yet the industry continues to obscenely claim they can’t afford the staffing and support needed to help contain the spread,” continued Adanjesus Marin. “It is imperative that the Legislature acts swiftly to make nursing homes safer for Rhode Island’s most vulnerable residents and hold the nursing home industry accountable by passing the Nursing Home Staffing and Quality Care Act.”