Important facts on monkeypox
With the rise in monkeypox cases around the nation and the White House’s declaration of a public health emergency, it is imperative that people are aware of what the virus is, the stigmatization of affected populations, how people can protect themselves, and what is still unknown about the virus…
September 2, 2022, 11:10 am
By Gerilou Ebrada
Coyote RI has been heavily engaged in community conversations with the Rhode Island Department of Health (DOH) regarding concerns of monkeypox and providing feedback. Bella Robinson, founder and executive director of Coyote, has actively been part of Zoom sessions with DOH advocating for and including sex workers in the conversation. Bella has asked sex workers what their take on monkeypox is and has relayed some of their comments and questions to healthcare officials representing DOH. Additionally, Coyote has been involved as part of a focus group on DOH’s monkeypox awareness campaign.
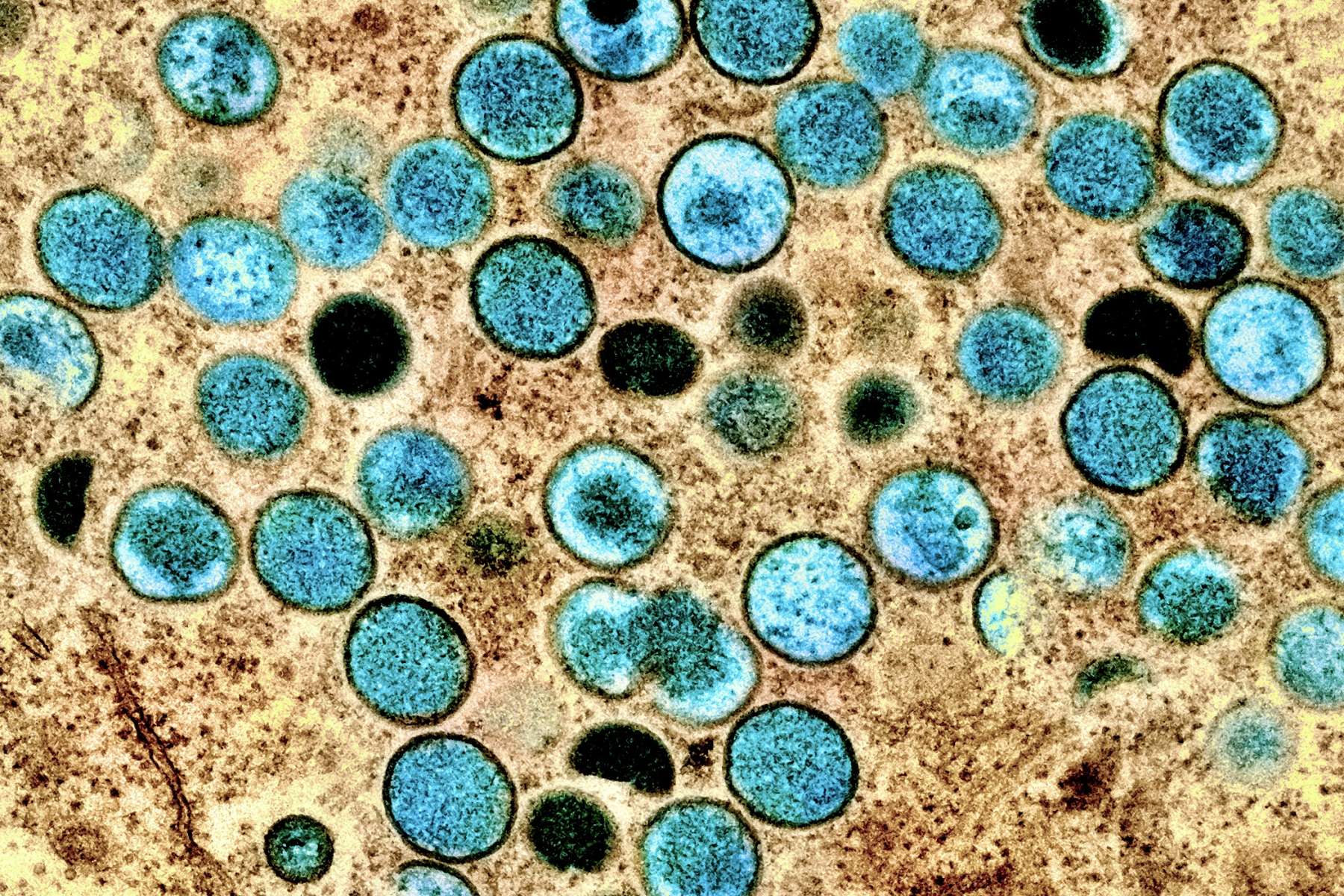
WHAT IS MONKEYPOX?
Monkeypox is a viral illness that shares symptoms similar to that of smallpox. The most notable symptom of the virus is a rash that can be located anywhere on the body (including the face, hands, feet, inside the mouth, and the genital area) and can present itself similarly to pimples or blisters. Along with the rash, people with monkeypox may also experience flu-like symptoms. According to infectious disease physician Dr. Phillip Chan, after exposure to the virus, it can take up to 21 days for symptoms to appear, so self monitoring after known exposure is extremely important. The Center for Disease Control states that a person carrying the virus is still infectious “until the rash has healed, all scabs have fallen off, and a fresh layer of skin has formed.” This process can take 3 to 4 weeks.
Monkeypox is primarily spread through direct contact with monkeypox sores, bodily fluids, contaminated items that have been in contact with infected sores, or respiratory droplets. As DOH concludes, the virus is sexually associated as transmission is typically due to close skin to skin contact with others who may be infected. Currently, the population most affected by the outbreak are gay, bisexual, and other men who have sex with men (GBMSM), as well as gender diverse people. However, anyone can become infected by monkeypox, including populations that engage in sexual acts with GBMSM or towels, bedding and other share items with the infected people. As a result, everyone must take the appropriate measures to protect themselves against monkeypox and healthcare providers must include sex workers, drug users, pregnant people, and the homeless as vulnerable populations at risk of the virus.
Recently, President Joe Biden ordered another 1.8 million vaccine doses to combat the outbreak. Initially, only 800k were ordered, but as cases rise, states have begun to demand more protection. Because of the small amount of vaccines available and the greater need, healthcare providers have begun to administer the Jynneos vaccine intradermally in order to get more out of the doses available. This change in vaccine administration demonstrates more aid needed in order to address what the White House deemed a public health emergency.
STIGMA
In a recent CDC review, 99% of monkeypox cases were men, the majority being MSM. Because of media depictions singling out GBMSM and people who have had multiple anonymous sexual partners, stigmatization similar to the AIDS crisis of the 1980s has resurfaced. Not only is stigmatization dangerous for the affected populations, but also for people outside of these populations. The focus on GBMSM, while much needed, may deter the general public from taking precautions in protecting themselves. Combining the stigmatization of monkeypox with the lack of resources and aid available to the general public, there are concerns of the virus spreading outside of the affected populations.
For example, a man from the United Kingdom contracted monkeypox after attending crowded outdoor events. He did not have sexual contact with anyone at these events, indicating that close contact with others who were infected caused the spread. Unfortunately, most media reports on the virus focus on sexual contact between GBMSM, leaving instances like these unheard.
Other vulnerable populations such as sex workers, the homeless, and drug users have been promptly left out of the conversation as well. For a virus labeled “sexually associated,” with bodily fluids and direct skin-to-skin contact being the main transmitters of the disease, excluding groups that are confronted with these factors daily is not only neglectful, but irresponsible. Tackling the populations most affected by monkeypox is important, but the efforts to contain the virus should include being vigilant of others who are equally at risk of contracting monkeypox.
INFORMATION WE OBTAINED BY ENGAGING WITH RI DOH
“We believe that monkeypox is largely being transmitted by close skin-to-skin contact during sex,” said Dr. Chan. “The available evidence, which reflects what we are seeing in Rhode Island, is that a lot of people have the rash on their genitalia which strongly suggests they got it from skin-to-skin contact in that area (up to 50%) when having sex. There is some evidence it is sexually associated; however, we also suspect it can be transmitted less commonly through other skin-to-skin contact, contact with (for example) linens, and less commonly potentially droplets. All this being said, if you are asking if we can prioritize cis-gender female sex workers (or any sex workers) for vaccination – I am open to discussing that possibility.”
Conclusions
DOH has updated the eligibility requirements to include sex workers and those who has had multiple anonymous sex partners in the past 30 days
Sex Workers Suggestions for RI DOH
- Continue to focus on sex workers, homeless people and at risk populations (could help curb spread)
- Education on what public should look out for- symptoms
- Education on how to protect oneself- risk factors
- Clarify quarantine guidelines
- Advocate for government assistance for those who need to quarantine
- Include risk factors for pregnant women in light of ROE
- Education on non sexual ways it can be transmitted, symptoms, cleanup protocols, and quarantine protocols.
- They also need to let the public know that the monkeypox vaccine “JYNNEOS” has been around for years and we know a lot about it, so it’s not like the COVID vaccines that were approved on an emergency basis
RESOURCES
- Disinfecting Home and Other Non-Healthcare Settings; Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 22 Aug. 2022
- Monkeypox: Last Week Tonight with John Oliver (HBO); YouTube, uploaded by Last Week Tonight, Aug. 8 2022
- Monkeypox Vaccine Interest Notification List; State of Rhode Island Department of Health,
- Texas reports death tied to monkeypox, a first in the U.S
- United States Monkeypox stats
Gerilou Ebrada is a COYOTE 2022 Summer Intern; John Jay College; 2023